DR can be asymptomatic for a long time, until significant damage to the retina occurs. The first symptoms may appear in one eye or in both eyes at once.
Pay special attention to:
• The appearance of doubling objects
• Blurry contours of objects
• Difficulty in reading any text
• The appearance of a shadow around objects
• The appearance of a dark spot in the field of view
• Violation of color perception
Risk factors
In order of importance, from most important to least important:
• Duration of diabetes mellitus:
• up to 5 years - frequency of occurrence 9-17%
• from 5 to 10 years - 44-80%
• from 15 years old - 87-99%.
• Inadequate glycemic control
• Uncompensated arterial hypertension
• High cholesterol
• Pregnancy
• Smoking
• Obesity, hyperlipidemia
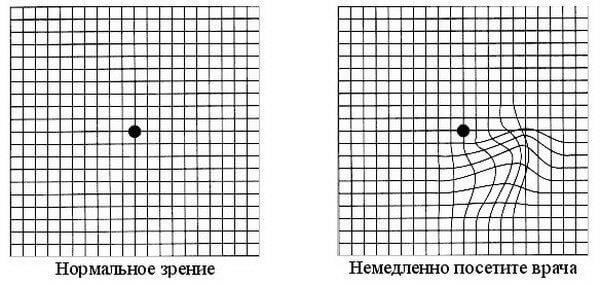
Anyone with diabetes is a potential patient with diabetic retinopathy. For self-control, regularly conduct an Amsler test
Stages of diabetic retinopathy
There are three stages, depending on the degree of damage to the retina:
• Stage I - Non-proliferative
• II stage - Preproloiferative
• III stage – Proliferative
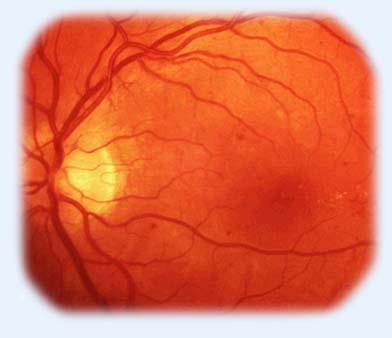
1. Non-proliferative diabetic retinopathy
Runs asymptomatic. When examining the fundus, you can see:
• Angiopathy - change in the caliber of blood vessels, expansion and tortuosity of veins
• Single solid exudates
• Microaneurysms
• Microbleeds
Methods of treatment
• Regular check-ups by an ophthalmologist - once or twice a year. Despite the fact that there is no decrease in vision, examination significantly reduces the development of complications such as macular edema, vitreous hemorrhage, retinal hemorrhage
• Adequate control of blood glycemia (!)
- • Compensation for concomitant risk factors for progression: arterial hypertension, cholesterol levels.
2. Preproliferative diabetic retinopathy
May be asymptomatic. There is a deterioration in the quality of vision: blurry contours, double vision, the appearance of a spot in the field of vision, a shadow around objects, difficulty in reading, impaired color perception.
Diagnosis reveals:
• Soft and hard exudates
• Intraretinal microvascular anomalies (IRMA)
• Severe angiopathy - looping of venules, changes in the caliber of blood vessels
• Multiple hemorrhages
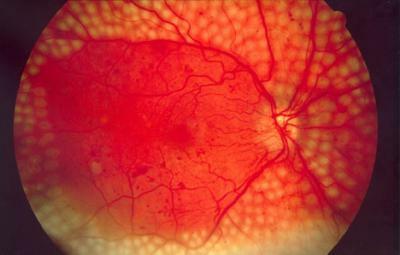
3. Proliferative diabetic retinopathy
The most severe form. It appears as:
a) Neovascularization - newly formed vessels, retinas, optic disc

b) Macrobleeds (preretinal, subretinal, subhyaloid, hemophthalmos) - there is a sharp decrease in eyesight, visual field loss, a dark spot in front of the eye.
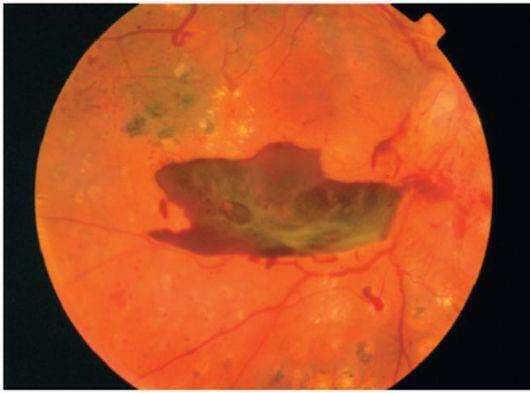
c) Gliosis
d) Traction retinal detachment
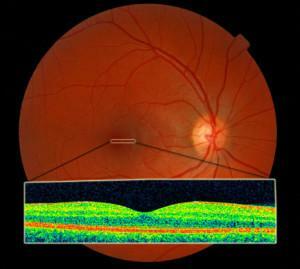
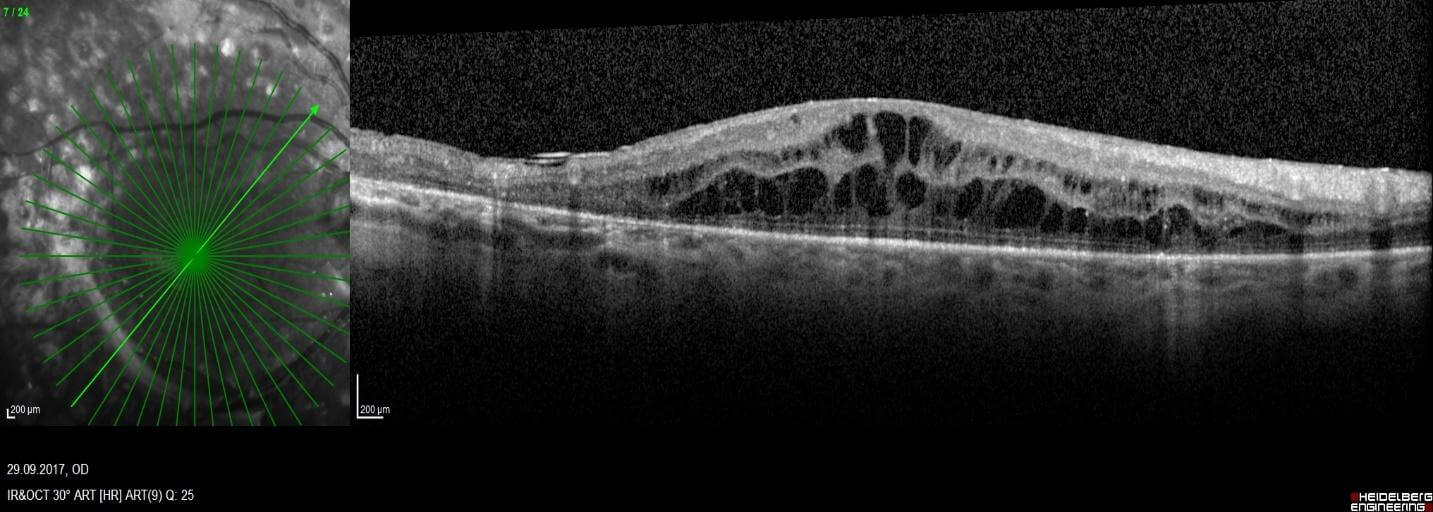
Diabetic macular edema
Can develop in all conditions. Accompanied by a sharp decrease in vision, "curvature" of straight lines and distortion of objects. Detected using optical coherence tomography.
Treatment of diabetic retinopathy
Treatment depends on the stage.
1. Профилактика
Золотой стандарт — панретинальная лазеркоагуляция сетчатки. Проводится при неосложненной ретинопатии в препролиферативную стадию. Значительно снижает риск развития осложнений и стойкого снижения зрения.
1. Prevention
The gold standard is panretinal laser coagulation of the retina. It is carried out with uncomplicated retinopathy in the preproliferative stage. Significantly reduces the risk of complications and permanent vision loss.
2. Treatment of diabetic macular edema
The patient is given intravitreal injections of anti-VEGF drugs and/or corticosteroids:
• "Eylea"
• “Lucentis|
• “Ozurdex”
3. Surgical treatment
In complicated forms of proliferative retinopathy (neovascularization, hemophthalmia, retinal hemorrhages, traction retinal detachment), surgical treatment is performed - subtotal vitrectomy, removal of proliferative tissue, endolaser coagulation.
Remember: the development and outcome of the disease depends on the stage. Since DR has no obvious symptoms and appears only after irreversible changes in the fundus, it is necessary to undergo routine examinations with an ophthalmologist.
And patients with diabetes should undergo it at least once a year!